Introduction to Childhood Pneumonia
While tremendous medical progress combats infectious diseases, pneumonia remains a leading killer of young children worldwide. Over 120 million cases surface annually in those under 5 years old, accounting for over 800,000 deaths. Understanding childhood pneumonia empowers parents and health providers to identify, promptly treat, and prevent this respiratory infection claiming so many young lives.
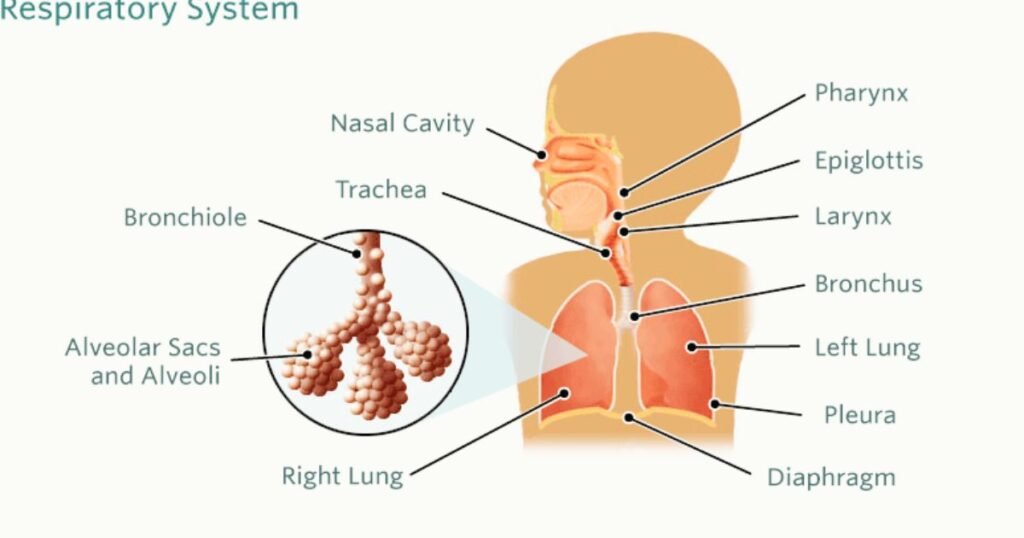
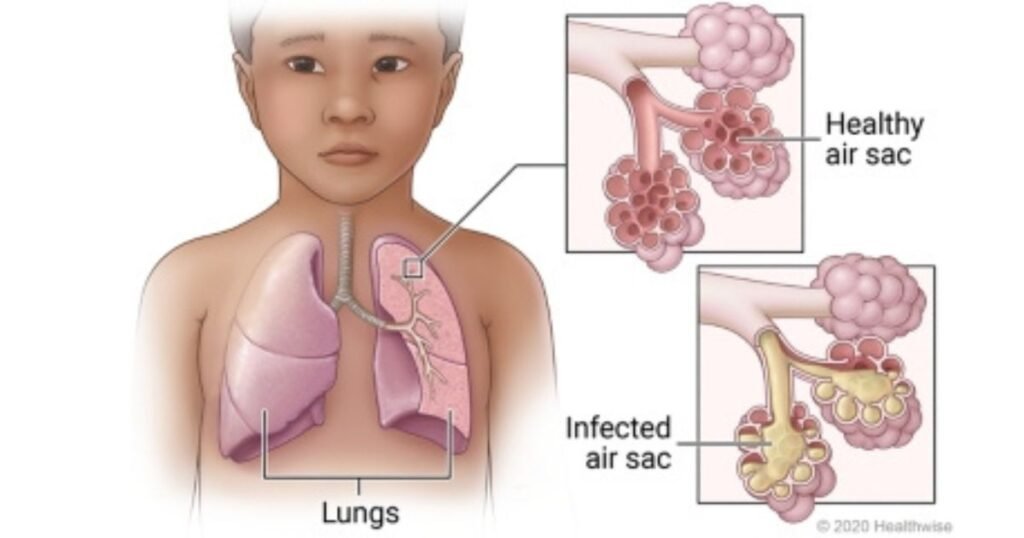
What is Pneumonia?
Pneumonia refers to an acute respiratory infection inflaming the microscopic air sacs in the lungs. Various bacteria, viruses or fungi can cause inflammation and fluid buildup that stiffens lung tissue and restricts oxygen circulation. Cells lining the airways also Childhood Pneumonia produce extra mucus further obstructing airflow. Risk increases in those with underlying heart/lung conditions or impaired immunity.
Read More:China Virus

Main Causes of Childhood Pneumonia
In children, pneumonia frequently results from these infectious organisms:
- Streptococcus pneumonia – Bacterial cause of most serious pneumonia cases globally. Spreads via respiratory droplets. Many strains now show antibacterial resistance.
- Respiratory syncytial virus (RSV)- Very contagious common virus triggering pneumonia in infants and younger children as immunity develops.
- Influenza – Flu viral strains often lead to bacterial coinfections causing pneumonia, especially in unvaccinated kids.
- Staphylococcus aureus – Increasingly prominent antibiotic-resistant bacteria provoking pneumonia.
- Haemophilus influenzae type B (Hib) – Leading bacterial pneumonia cause preventable by early vaccination.
Vaccines exist for pneumococcal, Hib and yearly flu pathogens cutting cases substantially. Boosting childhood immunization access lowers pneumonia mortality.
Childhood Pneumonia Symptoms
Symptoms develop when expanding lung inflammation restricts oxygen circulation. Common signs include:
- Rapid or difficulty breathing – Nasal flaring, retractions, wheezing, grunting
- Breathing faster than 60 breaths/minute indicates severity
- Cough producing phlegm or blood
- Fever – Though absent sometimes in very young
- Chills and chest pain
- Poor appetite, low energy, and confusion
- Blue tint to lips or nails in severe cases
Younger infants display less localized symptoms like poor feeding, vomiting, hypothermia, seizures or just seeming ill. Parents should seek urgent care with Childhood Pneumonia breathing difficulty or deteriorating condition.
Diagnosing Childhood Pneumonia
Doctors diagnose pneumonia based on:
- Confirming characteristic symptoms – fast breathing, chest wall retractions
- Medical history questions surrounding infections and vaccine status
- Physical exam checking oxygenation, listening to chest sounds
- Chest x-ray definitive for areas of lung inflammation though unnecessary for straightforward cases
- Microbiologic testing like sputum cultures to identify organisms in moderate/severe cases guiding treatment
Measuring oxygen saturation and counting respiratory rate help assess severity guiding inpatient versus outpatient therapy.
Treating Childhood Bacterial Pneumonia
- Oral or IV antibiotics combat bacterial pneumonia. Amoxicillin often first choice, while S. aureus/Influenza strains warrant tailored therapy.
- Fever/cough relieving medications make kids more comfortable.
- Oxygen supplementation until blood oxygen levels normalize.
- IV fluids prevent dehydration for kids unable swallow sufficiently
- Breathing treatments like albuterol nebulizers aid severe cases
- Antiviral medications may supplement treatment for viral coinfections
Most pediatric pneumonia cases resolve within 1-3 weeks with proper Childhood Pneumonia antimicrobial therapy. However prompt care is critical in severe pneumonia complicating smaller airways in young children.
Preventing Pneumonia in Children
Multiple prevention avenues exist to reduce childhood pneumonia contracting and dying from this infection:
- Breastfeeding babies strengthens initial immunity
- Comprehensive vaccination schedules prevent leading bacterial causes
- Treating/preventing HIV, malaria and malnutrition
- Reducing indoor air pollution through cleaner cooking fuels
- Preventing low birth weight which predisposes to infections
- Good hygiene like hand washing, sanitation, and reducing sick contacts
- Managing comorbidities like chronic lung disease, heart defects, diabetes
Global child health initiatives aim to increase protective factors while reducing risk exposures. Family education also ensures care seeking when warning signs appear. Childhood Pneumonia Through layered defenses, childhood pneumonia cases can be substantially reduced worldwide.
Conclusion
Pneumonia remains a preventable and treatable childhood infection. However education, vigilant monitoring, and access to care continue lagging in too many global regions. Tackling leading risk factors offers the best hope to protect vulnerable children from this devastating respiratory disease. Through quality medical care guided by parents and providers working together, kids worldwide are reaching their full potential no longer compromised by preventable illness.

Read More: Childhood Pneumonia
FAQs:
How can you tell a chest cold from pneumonia?
Colds feature runny nose and lower energy while pneumonia brings high fevers, rapid breathing, chest wall retractions. Doctors diagnose by exam, oxygen levels and x-ray.
Are pneumonia vaccines recommended for all kids?
Yes, full vaccination including annual flu and Polysaccharide vaccine at 2 years protects against leading pneumonia bacteria. Added coverage occurs in the 65+ pneumococcal vaccine.
Which kids face the greatest pneumonia risk?
Infants/toddlers with underdeveloped immunity and children suffering malnutrition, chronic diseases, or HIV are most vulnerable. Protective factors lower odds.
Can fungal infections also cause pneumonia?
Yes fungal organisms in soil/bird droppings can trigger rare cases when inhaled. Those with already suppressed immune systems are most prone. Prompt treatment cures fungal pneumonia.
Should I take my child to ER if pneumonia suspected?
Mild pneumonia can be managed by primary doctors with oral antibiotics. But difficulty breathing, low oxygen, or dehydration signals ER evaluation may be best for inpatient treatment.