Substance use disorders occur when frequent use of alcohol, opioids, stimulants, marijuana or other drugs impairs daily functioning, causes physical or psychological harm, and prompts ever-increasing use. About 40 million Americans ages 12 and older currently have a substance use disorder. Understanding the signs, risks, causes, treatment options, and roads to recovery empowers individuals and loved ones to take action against this destructive disease.
Signs and Symptoms
Signs of substance abuse versus dependence include:
Substance Abuse:
- Using drugs/alcohol in dangerous situations like driving
- Legal issues related to intoxication
- Relationship conflicts arising from intoxication
- Failing to meet work, school or home obligations
- Giving up social, work or recreational activities due to use
- Periodic alcohol/drug related injuries
- Continued use despite physical/psychological harm
Read More: Smoking Cognition
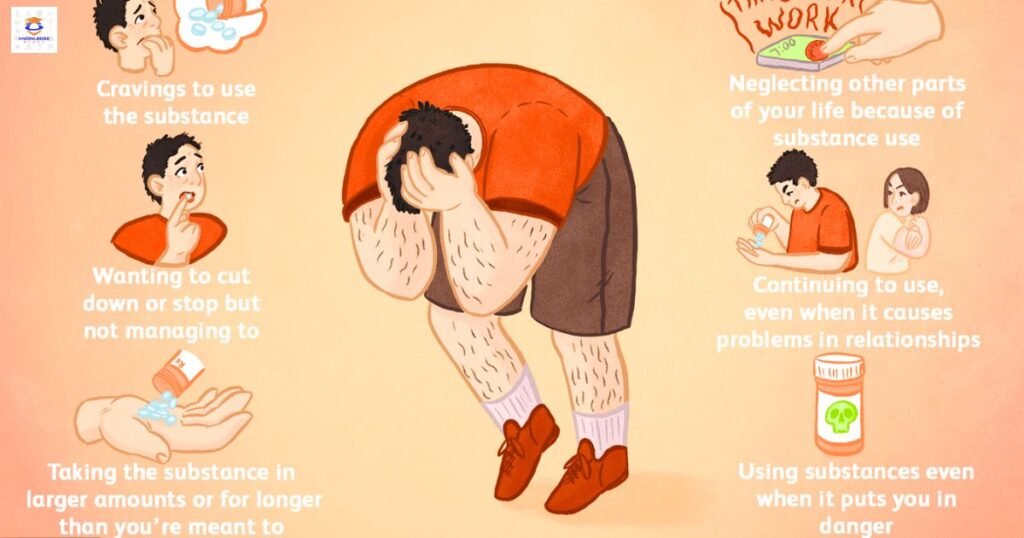
Substance Dependence:
- Drug tolerance – needing more to get the same effect
- Withdrawal sickness when not using
- Unable to quit or cut back use
- Significant time spent obtaining, using, recovering
- Inability to fulfill home, work, school responsibilities
- Social, work, or recreational activities given up
- Use continues despite physical or mental health effects
One pattern can evolve into the other. The more symptoms present, the more severe the substance use disorder.
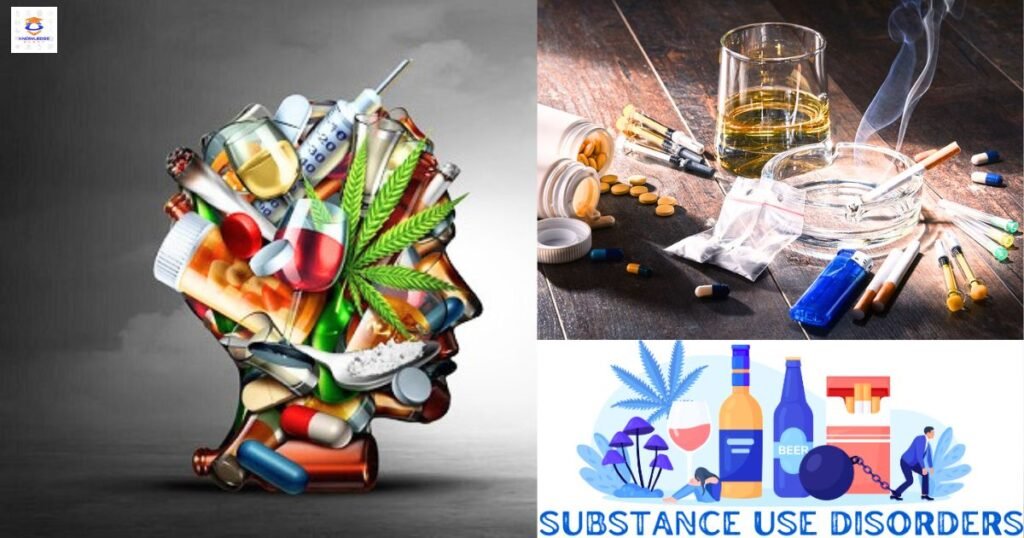
Most Commonly Abused Substances
While any substance has addiction potential, the most commonly abused substances include:
- Alcohol
- Opioids – Vicodin, OxyContin, heroin
- Cocaine, methamphetamine
- Cannabis – marijuana, hashish
- Sedatives – Valium, Xanax
- Hallucinogens – LSD, PCP
Concurrent use of multiple substances, known as polysubstance abuse, significantly increases health risks. Unprescribed use of legally obtained substances can also lead to addiction.
Causes and Risk Factors
Substance addiction is a complex disease with genetic, environmental, and social drivers including:
- Family history – Genetic predisposition to addiction
- Underlying mental illness – Coexisting conditions like anxiety, depression or PTSD
- Early exposure – Use during teen years when brains still developing
- Childhood trauma or abuse
- High stress lifestyle
- Peer pressure and social normalization of use
- Chronic pain or insomnia
- Lack of family/social support structures
- High accessibility and affordability of substances

Certain individuals have higher biological or social vulnerability to developing substance use disorders. Prevention efforts targeting youth focus on nurturing protective factors like positive social connections, life skills training, access to health care, and academic support.
Getting a Professional Evaluation
Seeking professional help is essential, but can feel intimidating. Many effective treatments exist, but finding the right approach hinges on an accurate diagnostic evaluation. Accredited treatment centers offer science-backed assessments providing insight into:
- Type, severity, duration and impact of substance use
- Coexisting medical or psychological conditions
- Motivations behind use and relapse triggers
- Barriers to stopping use like withdrawal risks
- Social/family dynamics that enable addiction
- Patient strengths, support structures, and recovery assets
Multidisciplinary input from psychologists, physicians, social workers, and nurses informs individualized treatment plans addressing all biopsychosocial elements perpetuating addiction. Evaluation removes assumptions, offers objective insights, and sets the stage for healing.
Treatment for Substance Use Disorders
Addressing the complex mental, physical, and social drivers perpetuating addiction requires an integrated approach including:
- Detoxification – Medically supervised detox allows safe alcohol/drug cessation minimizing dangerous withdrawal reactions. Often involves tapering medications.
- Behavioral counseling – Individual and group talk therapy builds coping skills, communication tactics, relapse prevention strategies, and addiction education. Cognitive, dialectical, and motivational approaches prove effective.
- Medication therapy – Medications relieve withdrawal symptoms, reduce cravings, or block addictive effects. Examples are disulfiram, methadone, buprenorphine, naltrexone. Allows patients to focus on recovery.
- Care coordination – Ongoing medical and mental health care ensures physical and psychiatric issues don’t jeopardize recovery.
- Social support – Peer support groups, family counseling, housing/vocational assistance establish alcohol/drug-free social connections and daily purpose.
Levels of care range from outpatient counseling to short-term residential to long-term therapeutic communities. Most utilize a “whole patient” approach recognizing substance addiction’s medical, psychological, and socially destructive impacts.
Recovering from Addiction
Overcoming substance addiction and remaining in recovery require physical detox followed by significant mental, emotional, and lifestyle changes over months to years. Recovery is a long-term process with ups and downs rather than an instant fix.
Relapse prevention relies on
- Establishing overall health and wellbeing
- Developing strong social and family support
- Avoiding people/places that enable past use
- Adopting substance-free leisure pursuits and hobbies
- Maintaining good self-care through nutrition, sleep, exercise
- Using learned coping strategies during cravings or emotional turbulence
- Having emergency preparedness plans if cravings intensify
Peer support groups, individual counseling, and sober living arrangements greatly aid the recovery process for many. Though addiction manifests differently in each person, countless individuals enter long-term recovery each year.
Conclusion
Substance addiction is a destructive yet highly treatable disease requiring intensive therapies and lifestyle changes. While the road is challenging, sustainable recovery is possible through medical detox, counseling, social support and relapse prevention education. Preventing first exposure among youth and improving access to integrated Substance Use Disorder treatment services helps loosen addiction’s grip on families and communities. Recovery brings immense personal rewards as lives once dominated by substances open to newfound health and purpose.
Read More: Substance Use Disorder
FAQs:
How do you know if someone has a substance use disorder?
Signs of use despite harm, giving up activities to use, habitual intoxication, escalating tolerance, withdrawal sickness, failed quit attempts indicate a substance use disorder.
What are common treatment options for drug addiction?
Detox, behavioral counseling, support groups, sober housing, medication therapies that relieve cravings or block Substance Use Disorder the addictive effect are common. Treatment should address medical, mental health, lifestyle, and social components.
Can someone completely recover after being addicted?
Yes, while addiction can always relapse if aftercare is stopped, many individuals are able to achieve full sobriety in which they maintain productive, purposeful lives without substance use.
What causes some people to become addicted while others won’t?
Biological factors like genetics, chemical sensitivity in one’s nervous system, and having another mental health condition contribute to addiction risk. Environmental factors also play a key role.
What happens if you abruptly stop alcohol or drugs after heavy use?
Depending on the substance, sudden cessation after prolonged heavy use can cause deadly seizures, stroke, heart attack, as the body goes into withdrawal. Medical detox supervision is imperative.





Autocad crack
Autocad 2025
autodesk autocad crack
auto cad crack
fl studio crack
fl studio 2025
idm crack
idm 2025
Internet Download Manager crack
revit crack
autodesk revit 2025
autodesk revit crack