Introduction
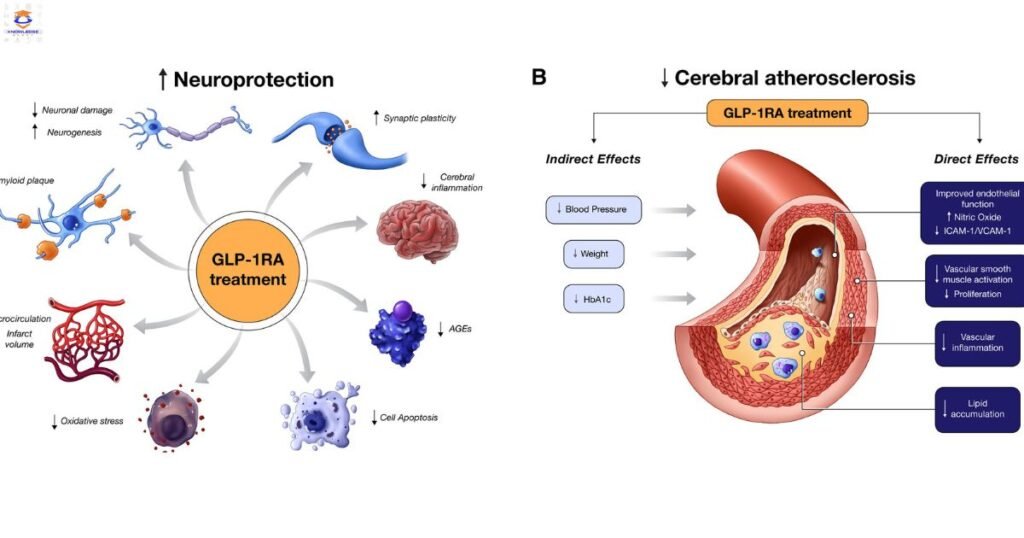
Glucagon-like peptide-1 (GLP-1) agonists are a class of injectable medicines used to treat type 2 diabetes. They help lower blood sugar levels by stimulating the release of insulin from the pancreas, suppressing glucagon secretion, slowing digestion, and increasing feelings of fullness. The American Diabetes Association recommends GLP-1 agonists as one of the treatment options for type 2 diabetes, especially in patients with established cardiovascular disease.
Guidelines for Prescribing GLP-1 Agonists
Before prescribing a GLP-1 agonist, confirm the diagnosis of type 2 diabetes and ensure the patient has not achieved their target blood sugar levels with lifestyle Prescribing GLP-1 Agonists changes and metformin alone. Check renal function, as GLP-1 agonists require dose adjustment or should be avoided in moderate to severe kidney disease. Assess cardiovascular risk factors like hypertension, history of heart attack or stroke. Those at high risk of heart disease may benefit the most from this class of medicines.
Read More: Knowledge Galaxy

Provide education on proper injecting technique, potential side effects like nausea and vomiting, the importance of adherence, and signs/symptoms requiring medical attention. Set blood sugar goals and a schedule for follow-up to monitor efficacy and tolerability. Start with the lowest effective dose and titrate slowly based on clinical response. Prescribing GLP-1 Agonists Combination therapy with other glucose-lowering agents may be required to optimize glycemic control.
Currently Available GLP-1 Receptor Agonists
There are several GLP-1 agonists approved as adjunct treatment for type 2 diabetes in the United States:
- Exenatide (Byetta, Bydureon) – twice daily and once weekly formulations
- Liraglutide (Victoza) – once daily injection
- Lixisenatide (Adlyxin) – once daily shot
- Semaglutide (Ozempic, Rybelsus) – once weekly injection or daily oral tablet
- Dulaglutide (Trulicity) – once weekly dose
The medications vary in their pharmacokinetics, with some having a shorter duration of action than others. Consider the patient’s lifestyle and preferences when selecting an appropriate GLP-1 agonist. Those desiring less frequent injections Prescribing GLP-1 Agonists may favor the once-weekly formulations.

Potential Side Effects
As with any medication, GLP-1 agonists have possible side effects:
- Gastrointestinal – nausea, vomiting, diarrhea are most common, especially early in treatment
- Hypoglycemia – when combined with insulin or sulphonylurea medications
- Pancreatitis – unlikely but requires prompt medical attention
- Injection site reactions – redness, swelling, irritation
Warn patients about these risks and report any severe or persistent symptoms to the prescribing physician. Fortunately, gastrointestinal effects normally improve over days to weeks of continued use.
Efficacy Considerations
A good response to GLP-1 therapy is defined as a reduction in A1c hemoglobin levels by 0.5-1.5% or more. Evaluate efficacy after at least 3 months of consistent injections. Patients with very high baseline A1c (>10%) are less likely to achieve Prescribing GLP-1 Agonists target goals with GLP-1 agonists alone. Consider combination approaches or transition to insulin if blood sugars remain uncontrolled after an adequate therapeutic trial.
Weight loss of 2-7% of body weight is an additional beneficial effect of this medication class resulting from reduced appetite and calorie intake. Obese patients may experience greater weight reductions. Ensure other causes of unintentional weight loss are ruled out.
Conclusion
GLP-1 receptor agonists provide glucose-lowering, weight loss, and cardiovascular benefits for many patients with type 2 diabetes. Follow prescribing guidelines to select appropriate candidates, provide education on proper use and potential side effects, set reasonable efficacy expectations, and monitor patients closely. Prescribing GLP-1 Agonists Combine with other agents if target A1c hemoglobin is not achieved. Used judiciously and safely, GLP-1 agonists can effectively improve diabetes outcomes.
Read More: Prescribing GLP-1 Agonists
Relevant FAQs
Q: How long until GLP-1 agonists start working?
A: These injectable treatments can begin lowering blood glucose within the first 1-2 weeks, but max glycemic effects may take up to 3 months.
Q: Can GLP-1 agonists be used with insulin?
A: Yes, combination therapy with basal insulin is an option for patients not achieving control with either medication alone. Prescribing GLP-1 Agonists This does increase hypoglycemia risk.
Q: Are GLP-1 agonists safe for people with kidney problems?
A: Dose reduction or avoidance is recommended for moderate-severe renal impairment. No dose adjustment needed for mild disease.
Q: Can GLP-1 agonists reverse type 2 diabetes?
A: No medication can reverse or cure this progressive condition. But started early, GLP-1 agonists can help Prescribing GLP-1 Agonists preserve pancreatic cell function.
Q: Are there any risks with stopping GLP-1 treatment?
A: There is no evidence of adverse effects from discontinuation. Prescribing GLP-1 Agonists Blood glucose and A1c levels will likely rise again without ongoing medication.