The human cardiovascular system is responsible for pumping blood throughout the body. It is made up of the heart, blood vessels and blood. The heart is a muscular organ that pumps blood through a network of blood vessels that includes arteries, veins, and capillaries. Blood vessels are responsible for carrying blood away from the heart and throughout the body. Blood is made up of red and white blood cells, platelets, and plasma, and is responsible for carrying oxygen, nutrients, and hormones to the body’s cells and removing waste products.
The heart has four chambers: the right atrium, which receives oxygenated blood from the body; the left atrium, which receives oxygenated blood from the lungs; The right ventricle, which pumps deoxygenated blood to the lungs for oxygen. and the left ventricle, which pumps oxygen-rich blood to the rest of the body.
The cardiovascular system works together with the respiratory system to deliver oxygen and remove carbon dioxide from the body. Oxygenated blood is pumped from the lungs into the left atrium of the heart and then into the left ventricle, from where it is pumped into the body. Deoxygenated blood returns to the right atrium, where it is pumped to the lungs for oxygenation.
The cardiovascular system also plays an important role in maintaining blood pressure and regulating blood flow to different parts of the body. Blood vessels contain smooth muscle that can constrict or dilate to control blood flow. The heart also has the ability to increase or decrease the rate of contraction to control blood flow.
Overall, the cardiovascular system is an important part of the human body that delivers oxygen and nutrients to body cells, removes waste products, and regulates blood pressure and flow.
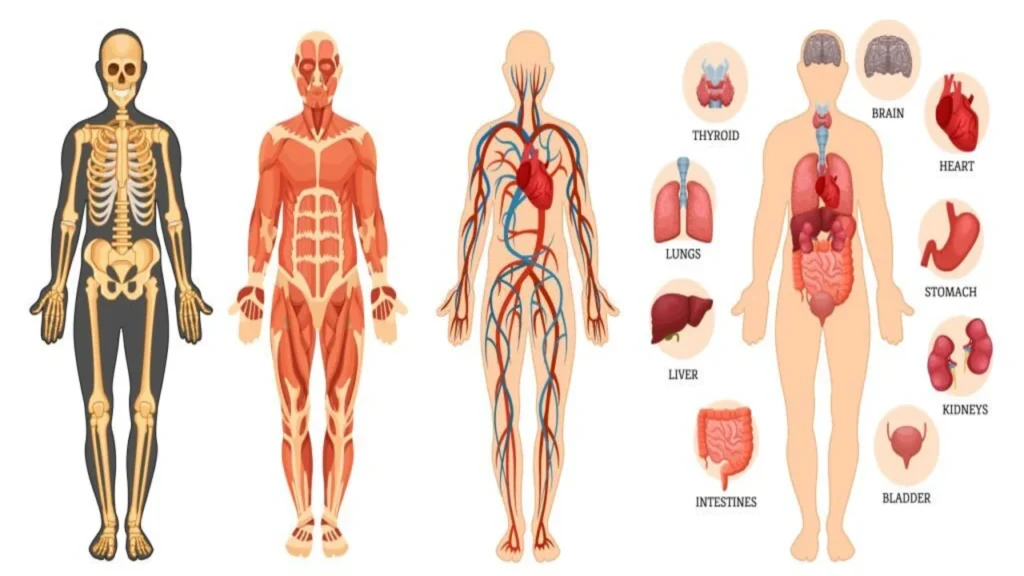
Cardiovascular System

Cardiovascular disease (CVD) refers to a group of conditions that affect the heart and blood vessels, including coronary artery disease, heart failure, valve disease, and peripheral artery disease. CVD is the leading cause of death globally and is caused by a combination of genetic, lifestyle, and environmental factors. Risk factors for CVD include high blood pressure, high cholesterol, smoking, diabetes, and a sedentary lifestyle. Treatments for CVD include lifestyle changes, medications, and procedures such as angioplasty and bypass surgery. It can be prevented by maintaining healthy lifestyle and regular check-ups.
Cardiovascular system May effect by Cardio vascular Diseases without any apparent symptoms. Many CVDs can develop at a time or lead to other diseases related to cardiovascular system.
The leading cause of death worldwide is Cardio vascular Diseases, approximately 17.9 million lives lost every year – This is 32 per cent of worldwide deaths.
History of Cardiovascular Disease
The history of cardiovascular disease (CVD) dates back to ancient civilizations with references to heart disease in writings from ancient Egypt, Greece and Rome. In these early writings, heart disease was described as a condition that caused chest pain and difficulty breathing.
During the Middle Ages, the study of CVD was largely limited to observations of symptoms and treatments focused on relieving symptoms rather than addressing underlying causes. In the 19th century, advances in medical technology, such as the stethoscope, allowed physicians to better understand the mechanics of the heart and blood vessels.
The relationship between diet and CVD began to be studied in the early 20th century. Researchers found that high amounts of dietary cholesterol and saturated fat can lead to a buildup of plaque in the arteries, known as atherosclerosis.
The development of heart-lung machines in the 1950s allowed the first open-heart surgery, and the 1960s saw the introduction of cholesterol-lowering drugs such as statins.
In recent years, the field of CVD research has expanded to include the role of genetics, inflammation, and lifestyle factors such as physical activity and stress in the development of CVD. Additionally, new treatments such as stents and angioplasty have been developed to open blocked arteries and prevent heart attacks.
In summary, the history of cardiovascular disease (CVD) can be traced back to ancient civilizations with references to cardiovascular disease in the writings of ancient Egypt, Greece, and Rome. In the 19th century, advances in medical technology, such as the stethoscope, allowed physicians to better understand the mechanics of the heart and blood vessels. The relationship between diet and CVD began to be studied in the early 20th century.
The development of heart-lung machines allowed the first open-heart surgery in the 1950s, and cholesterol-lowering drugs were introduced in the 1960s. In recent years, the field of CVD research has expanded to include genetics, inflammation, and lifestyle factors such as physical activity and stress in the development of CVD, and new treatments to open and prevent clogged arteries. has been prepared. Heart attack.
Major Causes of Cardiovascular Disease

As we have discussed earlier there is no apparent reasons of Cardio vascular Diseases. However, the primary cause of CVD is atherosclerosis- around the walls of the arteries the fatty plaques is build up. Fat, calcium, cholesterol and other substances build up plaques. Over time, blood flow is restricting as the arties get narrowed by hardening of plaque. It can block circulation of blood throughout the body.
ATHEROSCLEROTIC PLAQUE
Atherosclerotic plaque is of two types: stable and unstable.
STABLE ATHEROSCLEROTIC PLAQUE
As the plaque accumulated in arteries, the arteries get narrowed and blood flow is restricted, it can be diagnosed and treated.
UNSTABLE ATHEROSCLEROTIC PLAQUE
This type of plaque can rift, this may lead to blood clotting and they are big enough to barricade blood flow. Unstable Atherosclerotic Plaque is very hazardous, they can cause blockage of blood flow in the body without any warning. There is no diagnosis and treatment available still.
Cardiovascular Diseases
Common cardiovascular diseases are as follows:
- Acute coronary syndrome: blood supply to the heart is blocked
- Abnormal heart rhythms: Heart beats is irregular or rapid
- Heart failure: there is no working of heart. One type of heart failure is in which heart is not relaxed is “heart failure preserved ejection fraction (HFpEF). Based on National Health and Nutrition Examination Survey (NHANES) 2007-2010 in United States, age 20, about 5.1 million Americans have heart failure.
- Stroke: Arteries to the brain are blocked by blood clot, the blood supply to the brain is restricted and stroke is happen.
- Heart attack (myocardial infarction): there is no proper oxygen supply to the heart as the arteries are narrowed down. This is fatal.
- Congenital heart disease: This is by birth defect with heart structure; the most known type is single-ventricle congenital heart disease (Fontan-CHD).
- Preeclampsia: This is due to high blood pressure in postpartum period or pregnancy. It might be dangerous for both unborn baby and mother and can cause infant and maternal death.
- Rheumatic heart disease: Due to the infection of Streptococcal bacteria the Rheumatic fever damages the heart valves and muscle.
- Pulmonary embolism: blood clots from the veins of legs are moved to the lungs and heart and cause damage.
Cardiovascular Disease Symptoms

Cardiovascular disease symptoms and risk factors might be silent; this is silent killer for humans.
The most common symptoms of CVD with the heart or cardiovascular system include:
- Compression or chest pain around the chest area
- Blotting or nausea
- Discomfort and Fatigue
- Jaws, back and arms pain
- Shortness of breath
- Headedness or dizziness
- Cold sweats
- Frequently high blood pressure
- Vision fluctuations.
- Speaking trouble.
- Walking or balance issues
- Hypertension
- Sleep apnea
- Inflammation
These Symptoms might be different in women and Men. Women are more likely to show nausea and shortness of breath, Men are more likely to have chest pain.
HIV and Cardiovascular Disease (CVD)
HIV-infected individuals have rates of stroke and myocardial infarction. Smoking and diabetes are most common causes of cardiovascular and HIV.
Those men have higher risk of CVD and arteries plaque blockage who have long-term HIV infections rather than who have uninfected. Specifically, stenosis and plaque (narrowing of blood vessels) have been measured in patients of HIV infected patients.
In HIV-infected patients, CT angiography analyzed Non-calcified coronary artery plaque, high rate of heart attack, was more prevalent and extensive.
Cardiovascular diseases and obesity
We need fats for our balanced life but too many fats can lead to obesity and heart attack. As we have discussed earlier the fats are the responsible of heart attack. Fats are accumulated in arteries and become plaque that plaque blocks the supply of oxygen to the heart and the efficiency of heart is lower. Obesity can clog the vessels that may be the cause of heart attack and stroke. Exercise and weight loss can make heart life more for years.
Living with Heart Disease

Sanction yourself: What is your condition? Think actively about yourself, treatment options, and make valid steps to take successful treatment.
Frequent visits to clinics: ask your consultants the random question you have in your mind try to understand the precautions that healthcare provider told.
Trusted Healthcare provider: Take recommendations from your health provider and take a good decision about your health. Check the background of your consultant if you have any doubts then don’t go for your treatment and seek another trusted health provider. Going to untrusted health professional is fatal for your life.
Medication
ACE Inhibitors: stop blood vessels from narrowing, increase the amount of blood pumps in body. It increases the blood flow that is good for heart life.
Antiplatelet: when platelets (cells in the blood) stick together they cause clots in blood. It prevents the platelets from sticking.
Anticoagulants: it prevent to blood from clotting that are the major causes of Heart attack
Calcium channels blockers: ease workload of heart, it relax the blood vessels and increase the supply of oxygen to heart muscles.
Cardiovascular Renal Disease
Cardiovascular renal disease (CVRD) is a term used to describe the presence of both cardiovascular disease (CVD) and kidney disease (RD) in the same individual. CVD includes conditions such as hypertension, coronary artery disease and heart failure, while RD includes conditions such as chronic kidney disease (CKD) and end-stage renal disease (ESRD).
CVRD is a common and clinically important problem, as individuals with CVRD have a higher risk of death, hospitalization, and disability than individuals with CVD or RD alone. The two conditions share many risk factors, such as high blood pressure, diabetes, and smoking, and often occur together, meaning that the presence of one condition increases the risk of developing the other.
Management of CVRD is complex and requires a multidisciplinary approach involving cardiologists, ophthalmologists, and other health care professionals. Treatment usually includes specific treatment of risk factors such as hypertension and diabetes, as well as CVD and RD. Drugs such as ACE inhibitors and ARBs are commonly used to treat high blood pressure and preserve kidney function, while statins and antiplatelet agents are used to reduce the risk of cardiovascular events.
It is important to note that the term “cardiorenal disease” is often used to describe the coexistence of both CVD and RD, also known as “cardiorenal syndrome” and “renocardiac syndrome.” These terms are used interchangeably and refer to the same phenomenon.
Briefly, cardiovascular renal disease (CVRD) is a term used to describe the presence of both cardiovascular disease (CVD) and kidney disease (RD) in the same individual. CVRD is a common and clinically important problem. Yes, managing CVRD is complicated. And it requires a multidisciplinary approach that includes cardiologists, ophthalmologists and other health care professionals.
Cardiovascular Disease ICD 10

Cardiovascular disease (CVD) refers to a group of conditions that affect the heart and blood vessels. The International Classification of Diseases, 10th Revision (ICD-10) is a system used to classify and code diseases and injuries for statistical purposes. In the ICD-10 system, heart disease is classified into categories I00–I99, which includes circulatory diseases.
Some examples of specific CVD codes in the ICD-10 system include:
- I10 Essential (primary) hypertension
- I20-I25 Ischemic heart disease
- I30-I52 Other forms of heart disease.
- I60-I69 Mental illness
- I70-I79 Diseases of arteries, arterioles and capillaries
- I80-I89 Diseases of nerves, lymph vessels and lymph nodes, not elsewhere classified
- It is important to note that ICD-10 codes are used by medical professionals and insurance companies to evaluate and bill medical services. They are not intended for use by the general public to self-diagnose or self-treat any condition.
Briefly, cardiovascular disease (CVD) is a group of conditions that affect the heart and blood vessels. The ICD-10 system is used to classify and code diseases and injuries for statistical purposes. It consists of a series of codes. Which refers to heart disease and its subcategories.
Hypertensive Arteriosclerosis Cardiovascular Disease Sudden Death
Hypertensive arteriosclerosis is a type of heart disease (CVD) that causes thickening and hardening of the artery walls due to high blood pressure (hypertension). This thickening and hardening is known as arteriosclerosis, and it causes the blood vessels to narrow, making it more difficult for blood to flow through them.
Hypertensive arteriosclerosis can affect various organs and systems in the body, including the heart, brain, and kidneys. In the heart, it can lead to coronary artery disease (CAD), which can lead to angina (chest pain) and an increased risk of heart attack and heart failure. In the brain, it can cause cerebral palsy, which can lead to paralysis. In the kidney, it can lead to chronic kidney disease (CKD) and end-stage renal disease (ESRD).
Sudden death is a serious complication of hypertensive arteriosclerosis, particularly in the context of cardiovascular disease. Sudden cardiac death (SCD) is a term used to describe unexpected death from cardiac causes within an hour of the onset of symptoms, and is often caused by ventricular fibrillation, an abnormal heart rhythm. . Individuals with hypertension and CAD are at increased risk of SCD.
Hypertensive arteriosclerosis is a treatable and treatable condition. It can be prevented by maintaining a healthy lifestyle, including a healthy diet, regular physical activity, and not smoking. It can be treated with ACE inhibitors, ARBs and diuretics to lower blood pressure, as well as drugs to lower cholesterol and prevent blood clots.
In summary, hypertensive arteriosclerosis is a type of heart disease (CVD) that causes thickening and hardening of the artery walls due to high blood pressure (hypertension). Hypertensive arteriosclerosis affects various organs and systems of the body. Sudden death is a serious complication of hypertensive arteriosclerosis, especially in the context of cardiovascular disease, hypertensive arteriosclerosis is a treatable and treatable condition.
Is Asthma a Cardiovascular Disease

Asthma is a chronic respiratory disease characterized by inflammation and narrowing of the airways leading to difficulty breathing. It is not considered a cardiovascular disease (CVD), as it primarily affects the lungs and airways. However, there is a link between asthma and heart disease.
People with asthma have an increased risk of CVD, especially high blood pressure (hypertension) and heart failure due to a sedentary lifestyle. Furthermore, chronic inflammation in asthma may also contribute to the development of CVD.
Several mechanisms have been proposed to explain the link between asthma and CVD, including changes in the immune system, increased levels of inflammation, and changes in the levels of hormones and chemicals in the body.
Asthma can also affect CVD management. For example, asthma can make it difficult for individuals to exercise, which is an important component of CVD management. Additionally, some medications used to treat asthma, such as beta-adrenergic agonists and corticosteroids, can affect heart rate and blood pressure.
In summary, asthma is a chronic respiratory disease characterized by inflammation and narrowing of the airways. It is not considered cardiovascular disease (CVD), but there is a link between asthma and heart disease. It is more likely to happen. The possibilities are high. The risk increases. Especially high blood pressure (hypertension) and heart failure. The association is thought to be due to common risk factors such as obesity, smoking and a sedentary lifestyle.
Triglyceride HDL Ratio Prediction for Cardiovascular Disease
The triglyceride-HDL ratio is a simple and commonly used measure of cardiovascular disease (CVD) risk. Triglycerides are a type of fat found in the blood, while HDL (high-density lipoprotein) is often referred to as “good” cholesterol. The ratio of triglycerides to HDL is considered an indicator of overall lipid metabolism and can be used to predict CVD risk.
A high triglyceride-HDL ratio (greater than 4) is associated with an increased risk of CVD. This is because both high levels of triglycerides and low levels of HDL are considered independent risk factors for CVD. High triglyceride levels are associated with the development of fatty plaques in the arteries, which can lead to heart attack and stroke. On the other hand, low levels of HDL are associated with an increased risk of heart disease.
A low triglyceride-HDL ratio (less than 2) is associated with a reduced risk of CVD. This suggests that the person has a better lipid profile and is less likely to develop CVD.
It is important to note that the triglyceride–HDL ratio is only one of several risk factors for CVD and must be considered in the context of other risk factors such as age, sex, smoking, obesity, and family history. Should. Furthermore, it is important to note that the ratio is not a diagnostic tool, but a predictor of risk.
Finally, the triglyceride-HDL ratio is a simple and commonly used measure of cardiovascular disease (CVD) risk. A high triglyceride–HDL ratio (greater than 4) is associated with an increased risk of CVD, whereas a low triglyceride–HDL ratio (less than 2) is associated with a decreased risk of CVD, but age It should be considered in the context of Other risk factors include smoking, obesity and family history. Furthermore, it is important to note that the ratio is not a diagnostic tool, but a predictor of risk.
Statin Therapy for The Prevention and Treatment of Cardiovascular Disease

Statins are a class of drugs commonly used to lower blood cholesterol levels and reduce the risk of cardiovascular disease (CVD). These drugs work by blocking an enzyme called HMG-CoA reductase, which is involved in the production of cholesterol in the liver. By blocking this enzyme, statins reduce the amount of LDL (low-density lipoprotein) cholesterol in the blood, also known as “bad” cholesterol.
Statins have been shown to be effective in the prevention and treatment of CVD. They have been shown to reduce the risk of heart attack and stroke, as well as the need for bypass surgery or angioplasty. They have also been shown to reduce the risk of death from CVD.
In addition to their cholesterol-lowering effects, statins may also have anti-inflammatory and antioxidant effects that contribute to their ability to reduce CVD risk.
Statins are generally well tolerated and the risk of serious side effects is low. The most common side effects are muscle pain, weakness and fatigue, which can occur in up to 10% of people taking statins. These side effects are usually mild and can be managed by adjusting the dose or switching to a different statin.
Statins are usually prescribed to people who have high LDL cholesterol levels, a history of CVD, or who are at high risk of developing CVD. They are usually used in conjunction with other lifestyle changes, such as healthy eating, regular exercise, and weight management, to achieve optimal results.
In summary, statins are a class of drugs commonly used to lower blood cholesterol levels and reduce the risk of cardiovascular disease (CVD) by inhibiting an enzyme called HMG-CoA reductase, which breaks down cholesterol. breaks the Breaks down The liver is involved in the production of cholesterol, which lowers the amount of LDL (low-density lipoprotein) cholesterol in the blood, also known as “bad” cholesterol.
Statins have been shown to be effective in the prevention and treatment of CVD, reducing the risk of heart attack and stroke, as well as reducing the need for bypass surgery or angioplasty. They have also been shown to reduce the risk of death from CVD. Statins are generally well tolerated and the risk of serious side effects is low. They are usually used in conjunction with other lifestyle changes, such as healthy eating, regular exercise, and weight management, to achieve optimal results.
Cardiovascular Alzheimer’s Disease
Heart disease and Alzheimer’s disease have a complex relationship. Cardiovascular disease (CVD) is a group of conditions that affect the heart and blood vessels, such as coronary artery disease, heart failure, and stroke. Alzheimer’s disease is a progressive brain disorder that affects memory, thinking, and behavior.
There is evidence that CVD may increase the risk of developing Alzheimer’s disease, and that people with Alzheimer’s disease may also be at increased risk of developing CVD. For example, studies show that people with high blood pressure, high cholesterol and diabetes have an increased risk of Alzheimer’s disease. Similarly, people with Alzheimer’s disease have a higher risk of stroke or heart attack.
The underlying mechanisms linking CVD and Alzheimer’s disease are not fully understood, but researchers believe that inflammation, brain damage and other factors may play a role.
Read More: Human Brain Structure
It is important for people with CVD to manage their risk factors to prevent or delay the onset of Alzheimer’s disease. This includes maintaining a healthy lifestyle, such as eating a healthy diet, getting regular exercise, not smoking, and managing chronic health conditions. It is also important to keep your mind active by reading, writing and solving puzzles.
If you have any questions or concerns about the connection between CVD and Alzheimer’s disease, it is always best to speak with a health care professional. They will be able to provide you with more detailed information and guidance on how to manage your risk.
Cardiovascular Disease Picture




Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery disease (CAD) such as angina and myocardial infarction (commonly known as heart attack).
Cardiovascular disease (CVD) refers to a number of conditions affecting the heart and blood vessels, including coronary artery disease, heart failure, and stroke. These conditions can be caused by various factors, such as high blood pressure, high cholesterol, smoking, diabetes and obesity.
Symptoms of CVD can vary depending on the type of condition, but may include chest pain or discomfort, shortness of breath, fatigue, and an irregular heartbeat. Many people with CVD have no symptoms until an event such as a heart attack or stroke occurs.
It is important to understand that CVD is treatable and curable. Maintaining a healthy lifestyle, such as eating a healthy diet, exercising regularly, not smoking, and managing chronic health conditions, can help reduce the risk of CVD. Regular checkups with your doctor can also help identify and manage CVD risk factors.
If you have any questions or concerns about CVD, it is always best to speak with a health care professional. They will be able to provide you with more detailed information, including pictures and diagrams that may help you understand your condition.
Other CVDs include stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, abnormal heart rhythms, congenital heart disease, valvular heart disease, aortic aneurysm, peripheral arterial disease and venous thrombosis. The underlying mechanisms differ depending on the specific type of CVD. Risk factors for CVD include: high blood pressure, high blood cholesterol, smoking, diabetes, obesity, poor diet, lack of physical activity, and excessive alcohol consumption.
It is important to note that although asthma is a lung disease, it is not considered a heart disease. However, asthma and heart disease may have a complex relationship. People with asthma are at increased risk of heart disease and people with heart disease are at increased risk of developing asthma. Additionally, asthma can aggravate existing heart disease and vice versa. Therefore, it is important for asthma sufferers to manage their asthma and cardiovascular risk factors to avoid any complications.
Medical Approach to Cardiovascular Disease
Medical approaches to treating cardiovascular disease (CVD) include a combination of lifestyle changes and medications. The goal of treatment is to reduce the risk of heart attack, stroke and other CVD-related complications.
Lifestyle changes:
- Diet: A healthy diet low in saturated and trans fat, cholesterol, and sodium can help lower cholesterol and blood pressure levels and reduce the risk of CVD.
- Exercise: Regular physical activity can help reduce the risk of CVD by improving blood flow, lowering blood pressure and cholesterol levels, and promoting weight loss.
- Quit smoking: Smoking is a major risk factor for CVD, and quitting smoking can significantly reduce the risk of heart attack and stroke.
- Weight management: Maintaining a healthy weight can help reduce the risk of CVD by reducing stress on the heart and blood vessels.
Medicines:
- Cholesterol-lowering drugs (statins): These drugs help lower low-density lipoprotein (LDL) cholesterol levels, which can help reduce the risk of heart attack and stroke.
- Medicines that lower blood pressure (ACE inhibitors, beta blockers, diuretics): These medicines help lower blood pressure, which can help reduce the risk of heart attack and stroke.
- Antiplatelet medications (aspirin): These medications help reduce the risk of blood clots, which can help reduce the risk of heart attack and stroke.
- Diabetes medications: For people with diabetes, medications that help control blood sugar levels can help reduce the risk of CVD.
It is important to note that the specific treatment regimen will vary depending on the individual’s condition and risk factors. It is always best to speak with a healthcare professional to understand the best course of treatment for you.
Cardiovascular Disease Infographic

However, an infographic on heart disease may include information such as disease prevalence statistics, common risk factors (such as high blood pressure, high cholesterol, smoking, and obesity), and disease prevention and management. Ways to do it (such as eating a healthy diet, getting regular exercise, and taking prescribed medicines).
It may also include pictures or images of the heart and blood vessels to clearly understand the disease and its effects on the body. Some common signs and symptoms of heart disease may include chest pain, shortness of breath, and fatigue.
Cardiovascular Disease Dataset
There are many datasets available that contain information on cardiovascular disease. Some examples include:
National Health and Nutrition Examination Survey (NHANES) data set administered by the Centers for Disease Control and Prevention (CDC) in the United States. This dataset contains information on the health and nutrition of a representative sample of the US population, including data on cardiovascular risk factors and outcomes.
The Million Veteran Program (MVP) dataset is a partnership between the Department of Veterans Affairs and the Department of Defense. The dataset includes health and lifestyle information on more than one million veterans, including heart disease data.
The Framingham Heart Study dataset is a long-term study of heart disease risk factors that began in 1948. This dataset contains participant health and lifestyle information, including data on cardiovascular outcomes.
World Health Organization (WHO) Cardiovascular Disease Surveillance dataset, which includes information on cardiovascular disease prevalence and mortality in different countries of the world.
Atlas of the European Society of Cardiology (ESC) cardiology dataset, which contains information on cardiovascular morbidity and mortality in different European countries.
These datasets can be useful for researchers and health professionals to study cardiovascular disease trends, risk factors, and outcomes and develop strategies for disease prevention and treatment.
Pros & Cons of Human Cardiovascular System

The human cardiovascular system has several pros and cons:
Pros:
- The cardiovascular system is essential to sustain life by pumping oxygen and nutrients to the body’s cells and removing waste products.
- The heart and blood vessels are able to adapt to changes in the body’s needs, such as during exercise or pregnancy.
- The cardiovascular system helps regulate body temperature and fluid balance.
- The cardiovascular system is capable of repairing itself to some degree, such as through the growth of new blood vessels or the development of collateral circulation.
Cons:
- Cardiovascular disease is a major cause of morbidity and mortality worldwide.
- Risk factors such as high blood pressure, dyslipidemia, and smoking can lead to heart disease and can be difficult to control.
- Certain populations, such as diabetics, the elderly, and those with genetic predispositions, are at increased risk of heart disease.
- Heart disease can have serious consequences, such as heart attack, stroke and heart failure, which can lead to disability and death.
- Heart disease can be expensive to treat and may require lifelong medication.
Some treatments, such as bypass surgery or angioplasty, may have complications or are not suitable for some patients.
Overall, the human cardiovascular system is essential for sustaining life, but it is also highly susceptible to disease. Maintaining a healthy lifestyle and managing risk factors are important to reducing your risk of heart disease and improving your chances of living a healthy and fulfilling life.
Conclusions
The human cardiovascular system is a complex and important system responsible for pumping blood throughout the body. The heart is the main organ of the cardiovascular system, and consists of four chambers: right atrium, left atrium, right ventricle, and left ventricle. Blood is transported from the heart to the rest of the body by a network of blood vessels that includes arteries, veins, and capillaries.
Cardiovascular disease is a major cause of morbidity and mortality worldwide, with hypertension, dyslipidemia, and smoking being the most common risk factors. This disease can manifest in different ways, such as heart attack, stroke and heart failure.
Prevention and management of heart disease include lifestyle changes such as a healthy diet, regular physical activity and avoiding smoking. Statins and blood pressure-lowering drugs are also commonly used to reduce risk factors.
Finally, understanding the human cardiovascular system and the causes and consequences of heart disease is critical to the development of effective prevention and treatment strategies. Ongoing research on the cardiovascular system is essential to improving our understanding of heart disease and helping to reduce the burden of heart disease on individuals and society.