Introduction
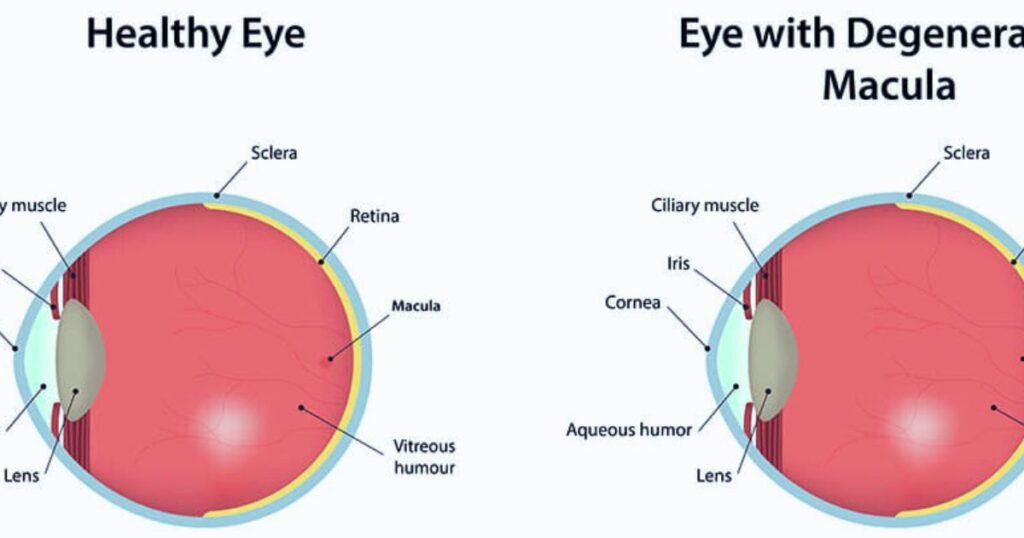
Macular degeneration is an eye disease that damages the macula, the central part of the retina responsible for sharp vision needed for activities like reading and driving. Age-related macular degeneration (AMD) is the most common form affecting people over 50. With the aging population, AMD prevalence is projected to double over the next 20 years, making understanding this progressive disease crucial.
Read More: SDN Ophthalmology
In this comprehensive guide, we’ll unpack the types, causes, risk factors, symptoms, diagnosis, and treatment options for macular degeneration. Keeping up with the latest knowledge empowers patients and physicians to slow AMD progression and protect sight.
Types of Macular Degeneration
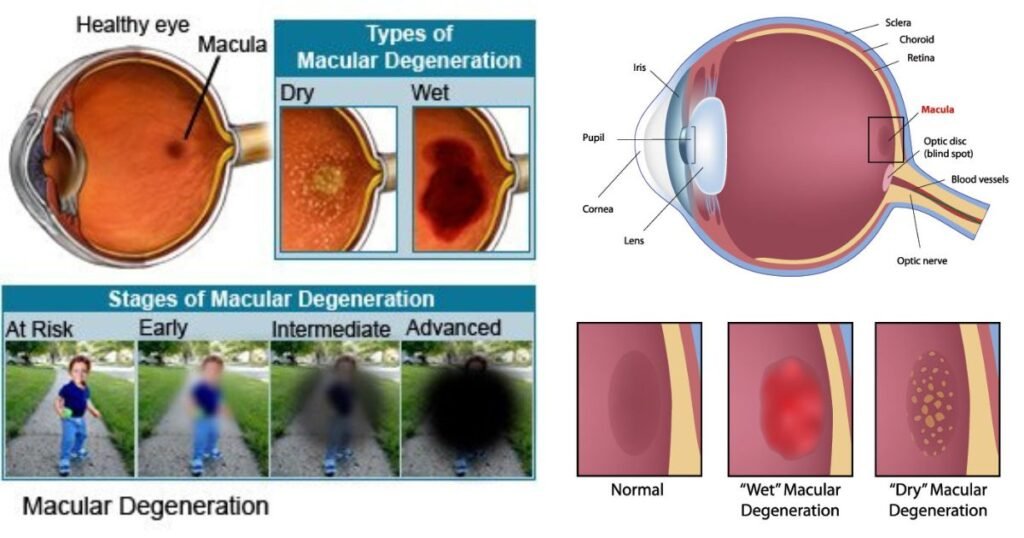
There are two main types of age-related macular degeneration:
Dry AMD – Dry AMD is the most common, making up 85-90% of cases. It develops when light-sensitive cells in the macula slowly begin to deteriorate. Small yellow deposits called drusen form under the retina between the retinal pigment epithelium (RPE) and Bruch’s membrane. While dry AMD often progresses gradually, advanced dry AMD can lead to vision loss.
Wet AMD – Wet AMD is more severe but less common, accounting for 10-15% of cases. It develops when abnormal blood vessels grow under the retina and macula, often due to advanced dry AMD. These vessels can leak fluid or blood called choroidal neovascularization (CNV), causing rapid damage. Wet AMD can cause drastic central vision loss within weeks or months if not treated.
Understanding the differences between dry and wet AMD is key for early intervention before major vision loss occurs.
Causes and Risk Factors
While AMD’s exact causes remain unclear, several risk factors are linked to its development:
- Age – Risk rises significantly above age 50 and continues increasing with age.
- Genetics – Gene variants associated with immune function and the complement system may increase risk.
- Race – Caucasians are more susceptible.
- Smoking – Smoking at least doubles risk of AMD.
- Sunlight exposure – May contribute to macular damage over time.
- Diet – Insufficient antioxidants, zinc, vitamins C and E, and omega-3s may be tied to AMD.
- Cardiovascular disease – High blood pressure and cholesterol correlate to higher risk.
- Obesity
- Light eye color – Blue eyes have higher sensitivity.
Knowing risk factors like age, genetics, and smoking status allows earlier screening and prevention.

Symptoms of Macular Degeneration
Early AMD may have no obvious symptoms. As it progresses, signs include:
- Blurred central vision – Distortion when looking directly at objects.
- Dark patches – Blind spots or empty areas in central vision.
- Color fading – Difficulty discerning colors or details.
- Crooked lines – Straight lines appearing wavy or crooked.
- Difficulty adapting to low light – Trouble seeing at night or in dim settings.
- Reduced contrast sensitivity – Loss of sharpness and detail.
If these vision changes occur, seek an eye exam immediately since early treatment is critical, especially for wet AMD.
Diagnosing Macular Degeneration
To diagnose AMD, eye doctors utilize:
- Visual acuity tests – Measure sharpness of vision using a Snellen chart.
- Dilated eye exam – Drops dilate the pupil to inspect the retina for signs of AMD.
- Tonometry – Tests fluid pressure inside the eye, which can increase with AMD.
- Imaging tests – Optical coherence tomography (OCT) produces cross-section retinal images showing AMD changes. Fluorescein angiogram detects retinal abnormalities and fluid leakage from wet AMD.
- Amsler grid test – Evaluates central vision by looking for gaps on a checkerboard pattern.
Based on exam results and imaging, ophthalmologists can determine if AMD is present and classify its stage to guide treatment.
Current Treatments
While no cure exists, several therapies help slow AMD progression and preserve vision:
- AREDS supplements – High doses of antioxidants and zinc may slow intermediate dry AMD based on the AREDS clinical studies.
- Anti-VEGF injections – Medications like ranibizumab (Lucentis) can treat wet AMD by blocking growth of abnormal blood vessels. Requires monthly injections into the eye.
- Photodynamic laser therapy – Laser destroys leaky blood vessels in some cases of wet AMD. Less common due to anti-VEGF efficacy.
- Monitoring – Tracking dry AMD progression with home Amsler grid monitoring and regular exams is important.
- Lifestyle changes – Quitting smoking, exercise, healthy diet, and UV protection may slow AMD progression.
Emerging research into stem cell therapy and retinal prosthetics aims to restore vision lost to macular degeneration.
Conclusion
Age-related macular degeneration threatens vision for millions of aging individuals globally. Knowing risk factors like smoking allows early screening and intervention to slow progression. Monitoring vision at home and undergoing regular eye exams help diagnose AMD in initial stages when treatment is most effective at limiting vision loss. While AMD remains incurable, persevering research brings hope for future therapies that may ultimately restore vision.

Read More: Macular Degeneration
Frequently Asked Questions
Q: At what age does risk of macular degeneration increase?
A: Macular degeneration risk rises above age 50 and progresses with age. Most patients are over 55 at diagnosis.
Q: How does wet AMD differ from dry AMD?
A: Wet AMD causes rapid vision loss from abnormal blood vessel growth under the macula. Dry AMD progresses slowly with retinal cell deterioration.
Q: What lifestyle changes can reduce AMD risk?
A: Quitting smoking, exercising, following a healthy diet rich in antioxidants and omega-3s, and limiting sunlight exposure may help.
Q: What are the first symptoms of macular degeneration?
A: Blurry or distorted central vision, dark patches in vision, and difficulty seeing at night or in low light are early symptoms.
Q: Can macular degeneration be cured?
A: There is currently no cure for age-related macular degeneration. But treatments like injections and supplements can slow progression and vision loss.