Introduction
Chest congestion is a medical condition that can make breathing difficult and cause discomfort. Congestion occurs when excess mucus clogs the airways, leading to wheezing, coughing, and shortness of breath. While congestion is often associated with colds and respiratory infections, many other factors can cause chest congestion. This article explores the causative factors, symptoms, and treatments for chest congestion to help you find relief.
Read More: Knowledge Galaxy
What Causes Chest Congestion?
There are several potential causes which results in this medical condition
Respiratory Infections
Respiratory infections like colds, flu, bronchitis, pneumonia, and COVID-19 often cause chest congestion as the body produces extra mucus in response to the virus or bacteria. This excess mucus clogs the airways, making breathing difficult.
Allergies
Allergic reactions to pollen, pet dander, dust mites, and other allergens can trigger chest congestion. The immune system sees these allergens as invaders. It releases histamine, causing inflammation and excess mucus in the lungs and airways.
Asthma
Asthma is a chronic medical condition described as narrowing and swelling of the lungs’ bronchial tubes. Irritants like smoke, pollution, and allergens can trigger asthma flare-ups and chest congestion.
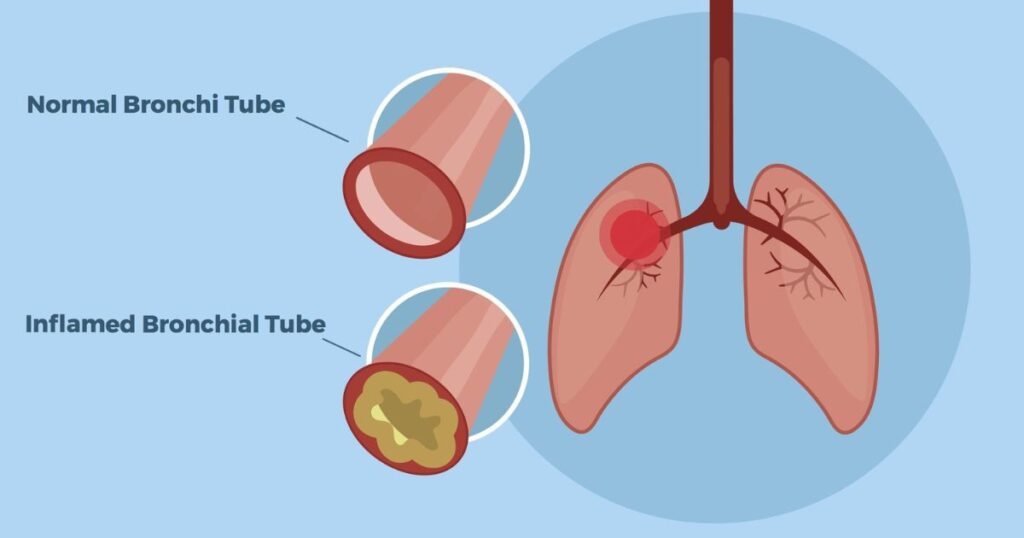
COPD
Chronic obstructive pulmonary disease (COPD) damages the lungs over time, making breathing difficult. COPD exacerbations often involve increased mucus production and chest congestion.

Environmental Irritants
Inhaling cigarette smoke, air pollution, chemical fumes, dust, and other irritants can cause temporary chest congestion as these agents inflame and clog the airways.
Heart Failure
When the heart cannot pump effectively, fluid can return to the lungs. This lung fluid leads to congestion, coughing, and shortness of breath.
What Are the Common Symptoms?
The highly common symptoms of chest congestion include:
- A productive cough produces phlegm or mucus
- Wheezing or raspy breathing sounds
- Tightness in the chest
- Shortness of breath
- Difficulty taking deep breaths
- Low energy and fatigue
- Runny nose
- Post-nasal drip
- Fever (with infections)
- Sore throat
- Headaches
- Muscle aches
In severe cases, symptoms may include a high fever, shaking chills, chest pain, a rapid heart rate, and coughing up blood. These require prompt medical attention.

How Is Chest Congestion Diagnosed?
To diagnose the cause of chest congestion, doctors typically:
- Take a medical history, asking about symptoms, risk factors, and potential exposures
- Perform a physical exam of the lungs and airways
- Use a stethoscope to listen for abnormal breathing sounds like wheezing or crackling
- Imaging tests like chest X-rays and CT scans
- Conduct pulmonary function tests to measure lung capacity
- Test mucus samples for bacteria or viruses
- Order blood tests to assess for underlying conditions
Treatment can be started while determining the root cause of congestion. Mild congestion often improves independently, while chronic or severe congestion requires medical treatment.
Home Remedies for Chest Congestion Relief

Several home remedies may help provide symptom relief for the mild congestion:
- Hot showers: Inhaling steam can moisturize and soothe irritated airways. Add eucalyptus oil for added decongestant effects.
- Saltwater gargling: Gargling with warm salt water helps thin out mucus and eases sore throat pain.
- Hydration: Drinking plenty of fluids keeps mucus thin and manageable. Hot teas may be especially soothing.
- Humidifiers: Dry air can irritate the airways. Use humidifiers or vaporizers to add moisture.
- Nasal irrigation: Rinsing the nasal passages (sinuses) with saline solution removes mucus and allergens.
- Rest: Getting extra rest allows the body to devote energy to fighting congestion.
- OTC (over-the-counter) medications: Decongestants, antihistamines, cough suppressants, and expectorants can all relieve congestion symptoms when used as directed.
Medical Treatments for Recurring Congestion
See a doctor if home remedies are not improving severe, chronic, or recurring congestion. Medical treatment options may include:

- Prescription cough medicines Contain higher doses of active ingredients than OTC products.
- Inhaled bronchodilators, Such as albuterol, open constricted airways, making breathing easier.
- Oral steroids: Reduce airway inflammation in conditions like asthma.
- Antibiotics: Prescribed for bacterial respiratory infections associated with congestion.
- Nebulizer treatments: Deliver fast-acting medication directly into the lungs to provide rapid relief.
- Oxygen therapy: Provides extra oxygen support to make breathing easier.
- Surgery: Procedures like a lung biopsy or removing obstructions may sometimes be required.
Lifestyle changes like avoiding smoking, improving indoor air quality, managing allergies, staying hydrated, and getting rest also help minimize the recurrence of congestion. Seek prompt medical care if severe symptoms persist or congestion persists for over a week.
This condition can be uncomfortable and frustrating. Identifying the underlying cause and using the right treatments can help relieve symptoms sooner. Contact your doctor if congestion is severe or interfering with daily life for prompt diagnosis and support. With the proper care, you can breathe easier again soon.
Chest Congestion FAQs
What’s the difference between chest congestion and a chest cold?
Chest congestion refers specifically to excess mucus buildup in the lungs and airways. A chest cold is an upper respiratory infection that can cause congestion and other cold symptoms like a sore throat, runny nose, and body aches.
Is chest congestion contagious?
Chest congestion itself is not contagious. However, some illnesses that cause chest congestion, like colds, flu, and COVID-19, spread easily from person to person through respiratory droplets. Maintaining good hand hygiene and having less contact with sick individuals reduces transmission risk.
How long does chest congestion last?
Symptoms usually persist for 1-2 weeks for mild congestion from colds or allergies. Severe, chronic, or recurring congestion related to asthma, COPD, or chronic bronchitis may last for weeks or months without proper treatment.
When should I see a doctor for chest congestion?
See a doctor if congestion persists beyond 7–10 days, comes back frequently, is accompanied by a high fever, wheezing, chest pain, trouble breathing, or coughing up blood. These may indicate a more serious health issue in need of medical treatment. People with asthma, heart disease, or lung disease should also promptly report worsening congestion.
What foods help with chest congestion?
Warm, soothing foods like chicken soup, ginger tea, honey, citrus fruits, and spicy foods may help thin mucus and relieve symptoms. Staying well hydrated also helps loosen congestion. Avoid dairy products, which may promote extra mucus production.
Can I exercise with chest congestion?
Mild exercise may help loosen mucus through deeper breathing. But take it easy, as overexertion could trigger severe coughing or shortness of breath. Avoid exercise altogether when feverish or fatigued. Stop right away if you have trouble breathing or feel dizzy.
Can chest congestion lead to pneumonia?
It’s possible. If lung congestion is not cleared effectively, bacteria can grow in the trapped mucus, potentially leading to a pneumonia infection. Getting adequate rest and medications to suppress cough and clear phlegm help lower pneumonia risk.
Are decongestants safe during pregnancy?
Most decongestants are not recommended during pregnancy, especially in the first trimester. Safer alternatives include saline nasal spray, humidifiers, steam, rest, hydration, and certain cough medicines. Talk to your OB-GYN about which congestion medications may be appropriate.
Can chest congestion cause a fever?
Yes, fevers are possible when congestion is due to a respiratory infection like pneumonia, bronchitis, a cold, or the flu. Fever means the body is fighting an active infection. Congestion from asthma, allergies, smoking, or environmental factors typically does not cause a fever.
When is chest congestion serious enough to go to the ER?
Seek emergency care if you experience difficulty breathing, a high fever, chest pain, a rapid heart rate, blue lips or nails, confusion, or are coughing up blood-streaked mucus. These may indicate a more serious health issue requiring hospital treatment.